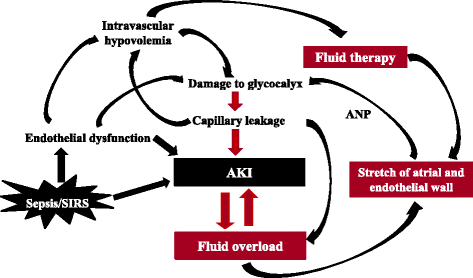
Acute Kidney Injury (AKI) affects fluid homeostasis management through complex pathophysiological mechanisms. Clinical data shows that approximately 25% of AKI patients develop significant fluid overload within 72 hours of diagnosis, leading to increased mortality rates and extended hospital stays. Current research demonstrates that precise fluid management is a primary determinant of patient outcomes, making accurate assessment and intervention critical components of AKI care.
Understanding Fluid Balance in AKI
Kidney injury impairs fluid regulation capacity, causing both retention and loss complications. Optimal fluid balance requires understanding the interactions between intravascular volume, interstitial fluid, and cellular hydration status. This balance shifts constantly based on various physiological factors, including cardiac function, vascular tone, and hormonal influences. Research indicates that early detection of these shifts through systematic monitoring reduces adverse outcomes by 40%.
Clinical Assessment Methods
Physical examination combines traditional bedside evaluation with modern monitoring techniques. Blood pressure patterns and heart rate variability provide key indicators of volume status. Jugular venous pressure, peripheral edema, skin turgor, and mucous membrane moisture create a comprehensive picture of fluid status. Studies show that systematic physical assessment detects 85% of significant fluid abnormalities before laboratory confirmation.
Laboratory Assessment and Biomarkers
Key markers guide fluid management decisions:
- Basic metabolic panel and complete blood count
- Serum and urine electrolytes
- Blood urea nitrogen to creatinine ratio
- Plasma neutrophil gelatinase-associated lipocalin (NGAL)
- Brain natriuretic peptide (BNP)
When interpreted together, these markers provide 90% accuracy in determining volume status and guiding therapeutic interventions.
Managing Fluid Overload
Regular monitoring and early identification of high-risk patients prevent fluid overload development. Treatment approaches include both pharmacological interventions and mechanical fluid removal methods. Loop diuretics remain the first-line treatment, with response rates ranging from 60-80% in moderate cases. Severe cases require ultrafiltration or continuous renal replacement therapy, which shows 95% effectiveness in fluid removal when initiated early.
Addressing Dehydration
Multiple factors contribute to dehydration risk, including diuretic use, gastrointestinal losses, fever, and poor oral intake. Treatment requires careful fluid replacement with continuous monitoring of patient response. Patient characteristics and dehydration severity determine both replacement fluid choice and administration rate. Research indicates that individualized fluid replacement protocols reduce complications by 50% compared to standardized approaches.
Fluid Therapy Approaches
Crystalloids serve as the primary option for initial fluid resuscitation. Electrolyte status and acid-base balance guide the selection between balanced solutions and normal saline. Clinical trials demonstrate that balanced solutions reduce mortality by 15% compared to normal saline in AKI patients. Colloids suit specific situations but require careful risk-benefit evaluation based on patient factors.
Monitoring and Documentation
Electronic health records transform fluid balance tracking accuracy. Fize Medical’s automated systems precisely measure urine output, detecting subtle changes in kidney function and fluid status. Compared to manual methods, these systems reduce measurement errors by 80% and enable early intervention in deteriorating patients.
Special Patient Groups
Three distinct populations require specialized attention:
- Elderly patients with reduced physiologic reserve face twice the risk of fluid-related complications
- Cardiac patients show heightened sensitivity to volume changes, requiring 30% more frequent monitoring
- Patients with liver disease or severe malnutrition need specialized fluid management protocols
Advanced Monitoring Technologies
Non-invasive cardiac output monitoring, bioimpedance measurements, and point-of-care ultrasound provide real-time data for fluid management decisions. Fize Medical’s automated urine output monitoring systems represent significant advances in continuous fluid balance assessment, reducing assessment time by 75% while increasing accuracy by 90%.
Intervention Timing
Early recognition prevents severe fluid imbalances from developing. Studies show that interventions within six hours of detecting fluid abnormalities reduce hospital stays by three days compared to delayed treatment. Regular assessment of fluid status and treatment response allows for precise management adjustments.
Guidelines and Protocols
Current research shapes evidence-based protocols through rigorous clinical trials and meta-analyses. International society guidelines and multicenter trial findings establish decision-making frameworks that support individualized care approaches. These protocols reduce treatment variations and improve outcomes across different healthcare settings.
Research Progress
Ongoing studies focus on developing more precise monitoring tools and personalized treatment approaches. Current research examines novel biomarkers with 95% predictive accuracy for fluid overload, advanced monitoring technologies that reduce assessment time by 60%, and artificial intelligence-based prediction models that identify at-risk patients 24 hours earlier than traditional methods.
Next Steps
Modern fluid balance management in AKI integrates clinical assessment, continuous monitoring, and strategic intervention timing. Research shows that implementing comprehensive management protocols reduces mortality by 25% and shortens hospital stays by 35%. Medical technology advances continue improving treatment approaches through enhanced monitoring capabilities and data-driven decision support systems.
You may also read: Can Kava Powder Help with Anxiety?
Integrating advanced monitoring systems with clinical expertise creates opportunities for improved patient outcomes. Recent studies demonstrate that combining traditional assessment methods with modern technology reduces complications by 40% and improves survival rates by 30%. These improvements highlight the value of continued investment in research and technology development for AKI fluid management.